How Humanoid AI Is Reshaping the Future of Hospitals, Surgery, and Patient Care
From surgical robots to hospital greeting machines, humanoid robots are significantly changing the healthcare industry. While not all healthcare robots have two arms and a friendly face, many combine mobility, perception, and interaction in ways that mimic human care staff. With a global healthcare labor crisis, an aging population, and rapid advances in AI and robotics, you get one of the biggest investment stories of the decade: from Tokyo to Texas, these machines are doing more than just turning heads, they’re turning the tide on staffing shortages, burnout, and ballooning healthcare costs.
At the heart of this revolution lies the convergence of several groundbreaking technologies—natural language processing, computer vision, tactile sensing, and cloud-based machine learning—that empower these robots to not only assist but sometimes outperform their human counterparts in speed, precision, and availability. In scenarios where healthcare professionals are overextended, these robots are stepping in to manage repetitive, physically taxing, or time-sensitive tasks, freeing human staff to focus on more complex care decisions.
But this transformation also raises a few issues around safety, ethics, cost, and how humans are forming relationships with their new nursing robots. Some of these issues may be able to be regulated, while others may pose additional challenges, such as building trust with patients, or working out issues relating to emotional connections with humanoids.
This isn’t science fiction. If you’re in healthcare, tech, or investment, pay attention: humanoid robots are about to transform one of the most labor-intensive and economically strained sectors in the world. The market implications are massive. Understanding this shift now means staying ahead of where policy, capital, and innovation are heading next, so let’s dive in. This report will cover:
- The scalpel and the smile: An overview of where humanoid robots are currently being used in healthcare, from surgery to companionship and mental health.
- Wired for bedside manner: A look at the technologies making it possible for humanoid robots to operate safely and effectively in clinical settings.
- Challenges to adoption: The key barriers to adoption, including trust, regulation, integration, and infrastructure.
- Investment in healthcare humanoids: Who’s funding the rise of medical humanoid robotics, including startups, Big Tech and public institutions.
- Case studies: Real-world case studies of humanoid robots at work in hospitals and care facilities.
- Bedside future: A forward look at what’s next, including generalist care robots, personalized AI caregivers, and global health deployments.
Let’s get started.
The Scalpel and the Smile: Where Humanoids Fit in Medicine
Humanoid robots are already being used in several cases across different medical, surgical, and therapeutic fields. With aging populations and overburdened health systems, humanoid robots are helping to fill critical gaps.
First, robotic arms have revolutionized minimally invasive surgery, and humanoid-inspired systems are increasingly present in the operating room. For example, CMR Surgical’s Versius features modular robotic “arms” that enable surgeons to perform precise, minimally invasive procedures by replicating the dexterity and range of motion of the human arm.

Figure 1: CMR Surgical. Versius robot.
Over 26,000 procedures have been performed with Versius, which makes it the second-most widely used platform after Intuitive Surgical’s da Vinci system, which itself has logged more than 10,000 units and over 14 million procedures globally.
The global market for surgical robotics is projected to reach US $14 billion by 2026. You can see in the US alone that the market is expected to reach around US$5 billion in the same period, as shown in the image below.
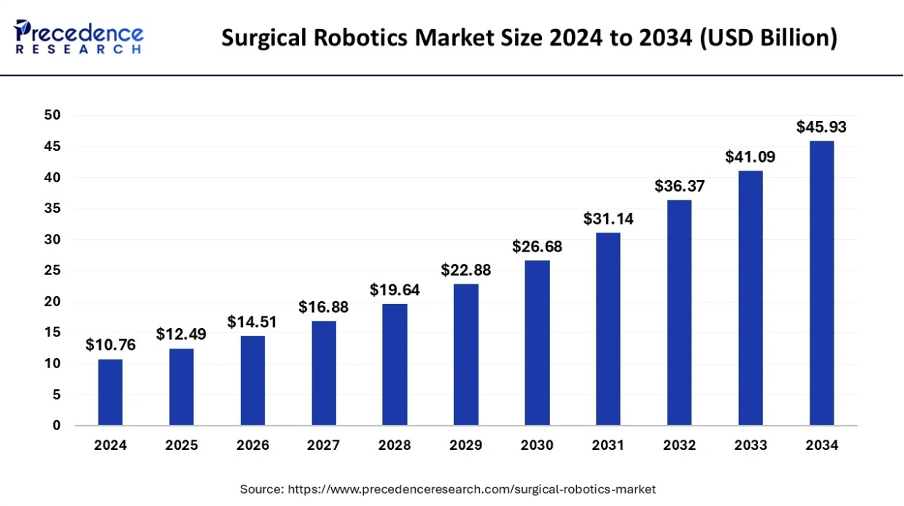
Figure 2: Precedence Research. Surgical Robotics Market Size 2024 to 2034 (USD Billion)
This projected growth is being driven by a combination of factors: a rising demand for precision medicine, increased investment in hospital automation infrastructure, and improved reimbursement policies for robotic-assisted surgeries in certain jurisdictions. Additionally, competition among manufacturers has begun to drive down costs, making robotic systems more accessible to mid-sized and regional hospitals. The result is a cascading effect that not only expands the market but democratizes access to state-of-the-art surgical care.
These types of surgical robots are not just widespread; they are also in some cases better than the humans that are using them. One study found that a “Smart Tissue Autonomous Robot (STAR), which is designed for complex soft tissue surgeries, can actually outperform expert surgeons on some key metrics.” This includes needle placement (which is done with more accuracy), and suture spacing, which is more consistent with robots.
These findings are not only remarkable for their technological implications—they signal a potential shift in the standard of care. In surgical environments where human fatigue, variability in hand precision, and inconsistent technique can affect outcomes, STAR-like systems promise consistent performance regardless of external pressures. Additionally, such robots can be pre-programmed to incorporate the latest clinical guidelines and adjust in real time using machine vision, thereby enhancing both precision and adaptability in ways human surgeons cannot always replicate.
Humanoid systems are also increasingly active in bedside care. The University of Hertfordshire’s Kaspar robot, designed for children with autism, and Hanson Robotics’ Grace, deployed in eldercare settings, both aim to build relationships with patients and support doctors and nurses. According to one report, around 60% of hospitals in developed countries already use robotic automation in some clinical form.
These robots go beyond mechanics—they are engineered to embody emotional intelligence. Grace, for instance, can monitor patients’ facial expressions and vocal tone to detect signs of pain or distress, adjusting its responses accordingly. In autism therapy, Kaspar’s consistent, non-threatening behavior pattern is ideal for encouraging social interaction in children who are often overwhelmed by human unpredictability. These applications highlight how humanoid robots can create emotionally safe environments that enhance treatment outcomes in sensitive populations.
In rehab clinics, humanoid systems are also helping with recovery timelines. Cyberdyne’s HAL exoskeleton used post-stroke, significantly improved patient recovery times. Chinese startup Fourier Intelligence is mass-producing their GR‑1 humanoid robot assistant, which can also help with carrying patients from beds to wheelchairs, and picking up objects. Over 100 units have already been deployed to different companies and organizations for testing.
In addition, logistics-focused humanoids are helping fill staffing gaps. Diligent Robotics’ Moxi operates in 30 U.S. hospitals, autonomously delivering meds, labs, and supplies. These tasks, although essential, are often time-consuming and prevent human staff from focusing on patient care. By taking over these duties, Moxi reduces human workload, lowers stress, and helps streamline hospital operations. Moxi operates autonomously and has already completed over 1 million deliveries in hospitals. This shows how robots could eventually handle much of the logistical support in healthcare facilities, allowing medical professionals to focus on more critical tasks.

Figure 3: Diligent Robotics. Moxi Robot.
Similarly, Aethon’s ZenaRX routinely delivers pharmacy samples, medication doses, meals, laboratory and surgical equipment or supplies, with 16 baskets in four compartments. Robots like this are multi-purpose and can help to reduce logistical loads on nurses and other hospital staff, which leaves them free to focus on patient care. Robots like the ZenaRX can operate for hours before charging.

Finally, companion bots like PARO (the robotic seal) are also being used to help patients in hospitals or care settings with stress. In one study ofdementia patients, PARO was perceived positively, with one patient stating “it’s like a buddy”, while another said “it makes me happy”. In pediatric units, NAO robots engage children during treatments, improving cooperation and reducing anxiety, as one study showed.
Emotional robotics represent one of the most profound intersections between healthcare and human psychology. While traditional therapy depends on human contact, these companion robots offer nonjudgmental, tireless interaction that some patients find easier to engage with. In long-term care, where loneliness and isolation are common, PARO’s lifelike responses—blinking, cuddling, reacting to voice—can provide meaningful emotional relief. Meanwhile, NAO’s programmable routines allow hospitals to tailor experiences to each child’s medical journey, using storytelling, games, and verbal encouragement to reduce fear and improve compliance. As these bots become more advanced, expect them to be used not just in care but also in early mental health intervention strategies.
Wired for Bedside Manner: Sensors, Software, and Smarts
Several different sensors, tools, and programming approaches are used by these robots to help them do their jobs in hospital settings. For example, understanding speech and responding with warmth isn’t easy. Robots use NLP and empathetic AI to figure out tone, intent, and micro‑expressions. Simulations based on neuromorphic and quantum-inspired models suggest humanoids of the future could replicate compassionate care by mimicking human emotional patterns.
In real-world settings, research on NAO robots shows that non-verbal signals, even including LEDs, can build trust and perceived empathy among elders in long-term care. In addition, a 2025 Axios article noted that 55% of 18–29‑year‑olds in the U.S. now feel comfortable discussing mental health with empathetic chatbots. As reported by BusinessWire in 2023, most doctors believe that AI chatbots will play a significant role within the next decade. Around 37% even stated that this would occur within the next 5 years:
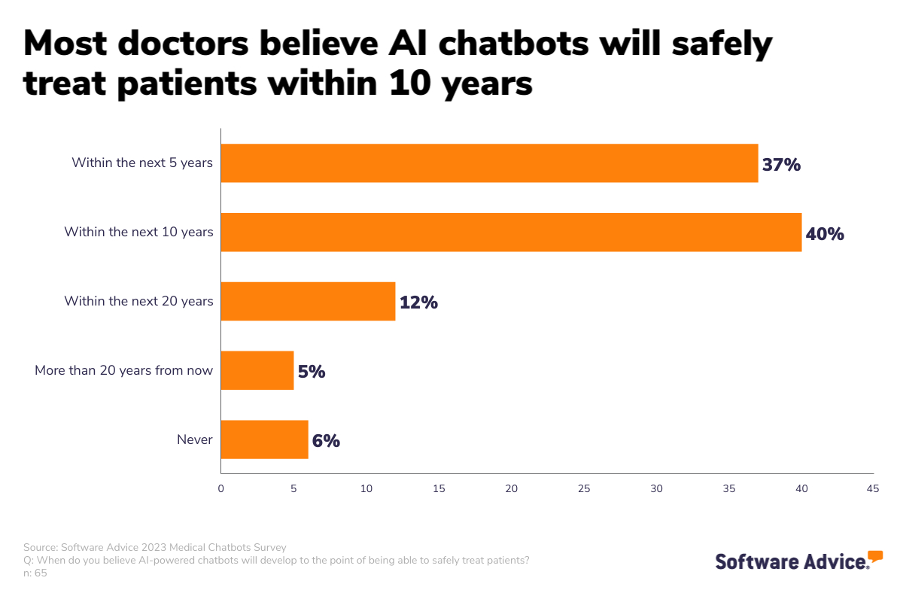
Figure 5: BusinessWire. Most doctors believe AI chatbots will safely treat patients within 10 years.
This generational shift is being accelerated by increasing digital fluency and mental health awareness. For many younger patients, talking to a digital entity removes the fear of stigma, judgment, or bureaucratic delay. Moreover, these systems can provide 24/7 interaction, keep detailed records for clinical use, and escalate complex cases to human therapists when necessary. As chatbot empathy models improve, we may soon see AI triaging mental health cases at scale, helping address the global shortage of psychological support in both urban and rural settings.
Additional sensors can provide feedback during surgeries, which is especially necessary in delicate procedures. In 2007, a Johns Hopkins team showed that adding force feedback to robotic systems significantly reduced suture breakage during cardiac surgery comparisons. Modern systems like the Shadow Hand guide remote operators with detailed touch-sensing. This allows safe telepresence in surgical and care tasks.
Force feedback, often referred to as haptic sensing, is now being embedded into next-generation surgical robotics to enable real-time tactile awareness. This allows surgeons to feel resistance, tension, and even subtle tissue textures through robotic interfaces—a game-changer in microsurgery and remote procedures. For instance, when conducting operations across long distances via 5G or satellite links, haptics ensures that human operators still have ‘touch-awareness’ even though they are physically separated from the patient. These systems are also being adapted for use in battlefield medicine and space missions, where human intervention is limited or delayed.
Integrated cameras, LiDAR, and multi-sensor fusion allow humanoids to detect facial expressions, monitor vitals, recognize gestures, and navigate space safely. The Pepper robot, for instance, combines speech, emotion recognition, and facial analysis to adjust interactions in hospitals. It can even detect anxiety and offer comforting words or activity suggestions.
Challenges to Adoption
While these humanoid robots provide a few benefits, there are also many barriers that stand in the way of real-world integration. First, getting a humanoid robot from lab testing to a hospital setting is expensive and slow. In the US, 510(k) submissions, which are for devices that are substantially equivalent to a legally marketed device, usually cost around $31 million and take about 10 months. Premarket Approval (PMA) submissions, which are for higher-risk devices, average $94 million and 4.5 years.
Regulatory fragmentation is another headache. The World Economic Forum notes that “the complexity of AI in health, inequitable access and fragmented, outdated regulations are some of the barriers that must be overcome for the potential of the technology to be realized.” An academic journal paper on the issue in 2024 also states that “it is still unclear whether and how healthcare robots in general are currently regulated.”
In countries with overlapping regulatory bodies—such as the FDA, FCC, and CMS in the United States, or the EMA and national health agencies in Europe—robotics companies must navigate a maze of overlapping and occasionally conflicting guidelines. Additionally, the lack of a global standard for medical robotics means that companies often must customize their robots to comply with local laws on data protection (like GDPR), AI transparency, and electrical safety, increasing costs and delaying international scaling.
Legal issues abound: if a robot makes a mistake, who is at fault? The designer of the robot, the developer of the code, the hospital, or the medical professional? Especially as robots may be integrated with healthcare systems regarding patient information as well, privacy compliance issues around healthcare data could become complex. Perhaps the same rules governing driverless cars can be applied to HC robots?
This legal gray area has already led to the emergence of robotic malpractice insurance policies, particularly for autonomous systems used in high-stakes procedures. Furthermore, legal scholars are now pushing for the concept of “AI personhood” or shared liability frameworks, where responsibility is proportionally distributed across stakeholders depending on the level of human involvement. Until such models are adopted, risk aversion among hospitals may prevent large-scale deployment—even when the technology is proven to be effective.
Furthermore, many patients and clinicians remain skeptical of humanoid robots, including fears around their safety, as well as their efficacy. A Pew Research study from 2022 found that more than half of Americans felt uncomfortable about the use of AI for healthcare purposes. While humanoid robots do not all use AI, the integration of these tools (and the skepticism around them) is linked, particularly in more vulnerable areas such as health and medical applications.
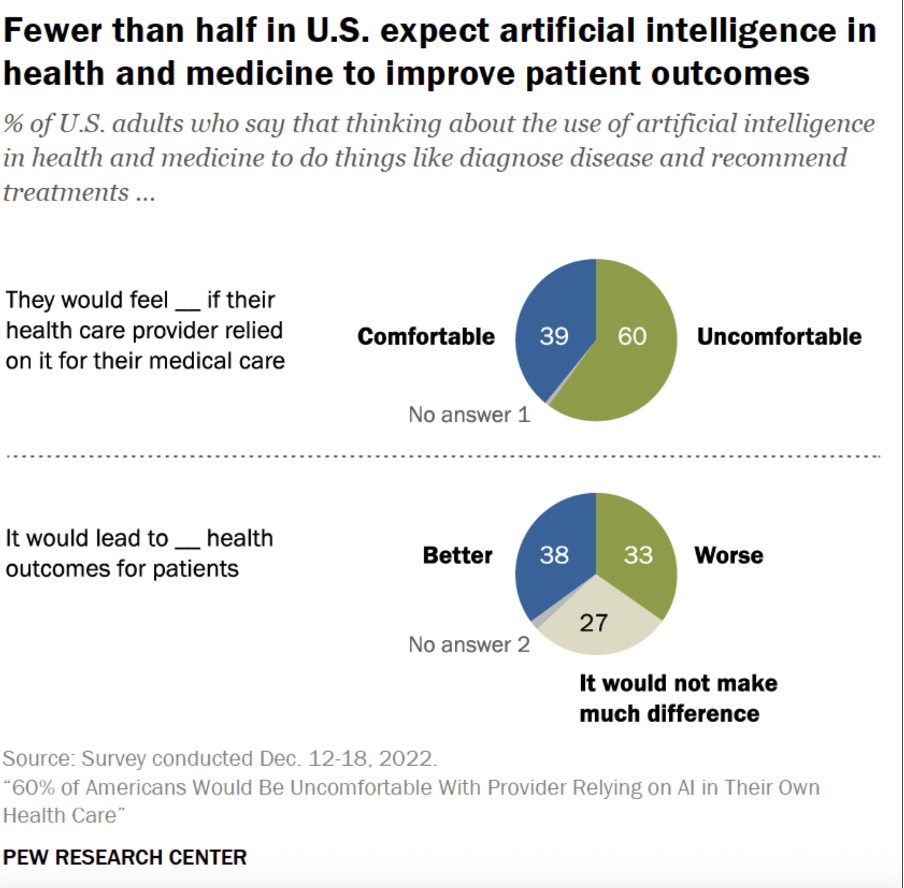
Figure 6: Pew Research Center. Fewer than half in U.S. expect artificial intelligence in health and medicine to improve patient outcomes.
A similar Pew study from 2017 found that the idea of “robot caregivers elicits a nearly equal mix of worry and enthusiasm: 44% of Americans are at least somewhat enthusiastic about this development, while 47% express some level of worry”. In contrast, a survey from Porsche Consulting found that “three out of four people in Germany would have no objection to being operated on by a robot instead of a surgeon at hospitals,” particularly if the risk of the operation being performed robotically was lower.
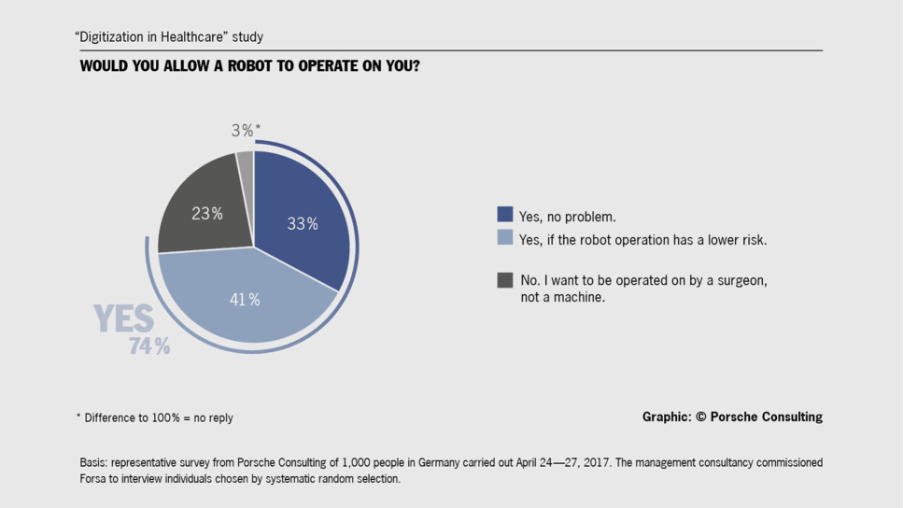
Figure 7: Newsroom. Would you allow a robot to operate on you?
These regional contrasts highlight how cultural attitudes, historical healthcare experiences, and media narratives can shape perceptions of robotic care. In Germany and Japan, where engineering and robotics are seen as integral to national identity, public trust tends to be higher. In contrast, in the U.S. and UK, where concerns about privacy, job loss, and inequality loom larger, public acceptance tends to lag—despite similar levels of exposure to the technology.
Ethical issues also include questions around autonomy (robots shouldn’t override human choice), informed consent, and emotional consequences. Some cases already show issues, such as a boy who became emotionally attached to an AI companion, and committed suicide as a result. These instances could also occur with humanoid companion robots, if not regulated and monitored carefully, with accompanying protective developments to the design of the robot. Medical “black-box” AI is another trust issue, as medical professionals must be able to understand and explain robot decisions.
In addition, robots can’t just be plugged in and instantly help. Instead, they need extensive staff training to use them, and to include them in hospital processes. Integration can be another problem: just because hospitals purchase the robot, it doesn’t mean it’s useful or even used.
This has led to the rise of specialized robot adoption teams and in-house roboticists within large hospitals. These teams work on customizing workflows, integrating with hospital IT systems, and providing hands-on support to clinicians. Training isn’t just technical—it includes modules on patient communication, ethical use, and emergency protocols. Hospitals that skip this integration phase often see expensive robots sitting idle in storage rooms, highlighting the gap between acquisition and application.
Finally, reliable digital infrastructure is necessary for their use: Wi‑Fi dead zones, cybersecurity issues, privacy problems, cloud storage and other digital issues can reduce the usability of an otherwise functional device. Additional costs for these aspects of performance can make these types of technologies prohibitively expensive for rural or under-resourced regions, leaving already-vulnerable areas further behind.
Investment in Healthcare Humanoids
Despite the many hurdles, several investors are focusing on humanoid robots in the healthcare sector as an opportunity. For instance, CMR Surgical (UK) recently raised an additional $200 million from backers, and is pursuing a sale of the business for about $4 billion. Its Versius system has facilitated over 30,000 procedures across more than 30 countries.
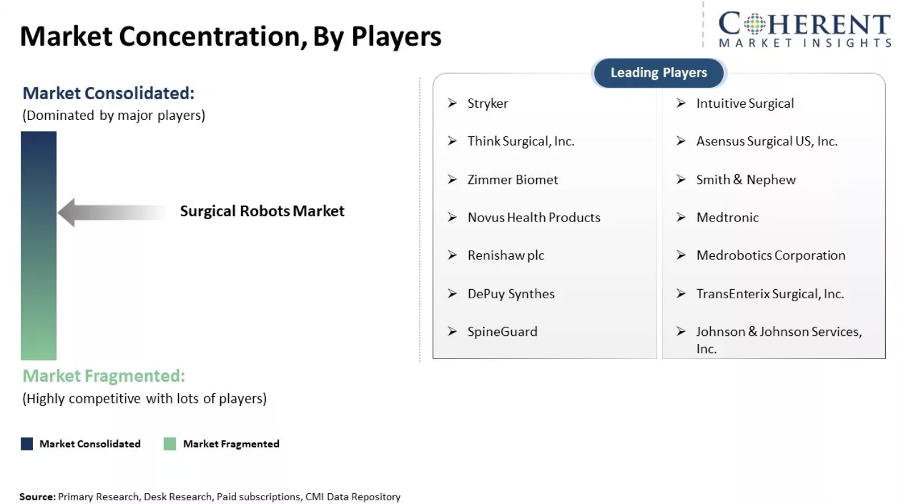
Mendaera (US), which produces a handheld, interventional platform, which combines robotics, AI, real-time imaging, and virtual connectivity, recently closed a $73 million Series B round of funding. Neura Robotics, which makes the humanoid 4NE-1, also secured €120 million in January 2025. Venture capital investment into robotics companies has been high over the past few years, with investment in the medical industry one of the largest areas. As shown in Figure 8 below, Coherent Market Insights notes that the surgical robot market is neither highly concentrated nor particularly fragmented, with several leading players such as Stryker (which makes surgical robotic arms) and Think Surgical (making knee replacement surgery robots).
Figure 8. Coherent Market Insights. Market Concentration, By Players.
Fox Corporate Finance’s Q3 2024 robotics report notes also that medical robots dominate when it comes to robotics sector deal count and volume. In the image below you can see that ‘Industrial Robots’ and ‘Medical Robots’ are the largest sub sector by deal volume. Some of this is due to mega funding rounds of CMR Surgical (€878m), with FCF noting that “CMR Surgical dominates the Top 10 list in the Robotics sector with 3 high volume deals” between 2019 and 2024. In Europe, they also note that “60% of the companies in the Top 10 are engaged in the subsegments Medical Robots or Industrial Robots, which emphasizes the maturity of & focus on these sectors.” Deal count over time for medical robots has also remained steady over the last years, with around 30-40 deals per year on average.
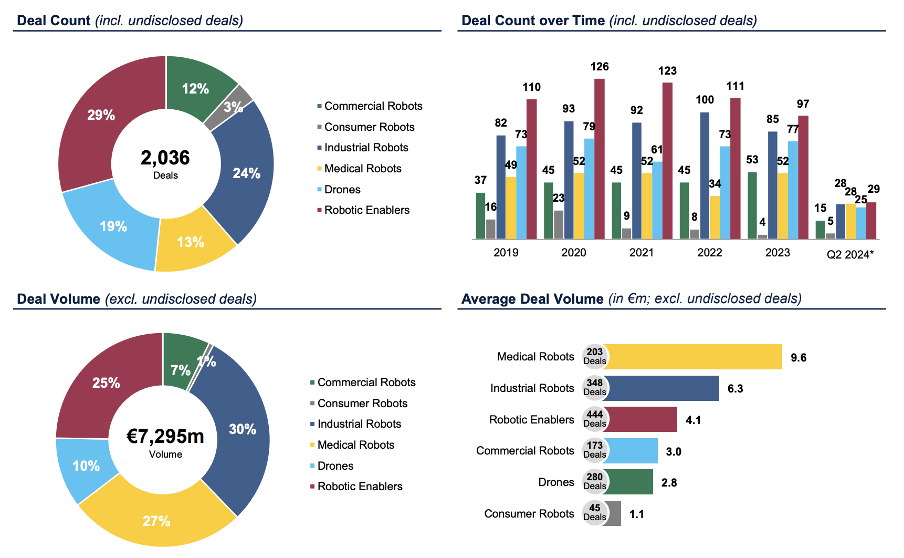
Figure 9: Fox Corporate Finance. European Robotics Subsector Analysis (‘19 – Q2 ‘24*).
Some startups have also made waves with innovative technology, such as ForSight Robotics, which has created a robot made specifically for eye surgeries. As reported in Forbes, they recently landed $125 million (USD) in funding led by Eclipse Ventures, to develop their technology Oryom, a world-first robotic technology for cataracts.
Other startups like Moon Surgical, backed by Sofinnova Partners and the venture capital arms of Nvidia and Johnson & Johnson, are challenging big players like Intuitive Surgical. Moon Surgical obtained FDA clearance for their commercial surgical robot last year.
Crunchbase notes that in 2024, “two of the biggest investments went to MMI, a developer of technology for robotic-assisted microsurgical procedures, and Capstan Medical, which is working on robotics-enabled technology offering a less invasive alternative to traditional open heart surgery. Both raised $110 million Series C rounds.” While these technologies aren’t of the humanoid variety, they highlight the growing interest in robotic medical technologies and their increasing integration in the sector.
Certain types of healthcare robots are also becoming more common as societal pressures and governmental decisions drive adoption. For example, the elderly care-robotics market is also expanding at a 20–24% CAGR across North America and Asia, which highlights VC shifts into social-care robotics.
Japan and South Korea, confronting ultra-aging populations, are promoting the use of elderly-care robots to provide solutions in healthcare, leading to increased investment. Reuters reported on this topic, highlighting the words of some care-facility leaders. “We are barely keeping our heads above water and in 10, 15 years, the situation will be quite bleak,” said Takashi Miyamoto, a director at Zenkoukai, an operator of elderly-care facilities. “Technology is our best chance to avert that.”
Real-World Case Studies
A few real-world case studies highlight the usefulness of these types of robots.
As noted, CMR Surgical’s Versius is a prime example of humanoid technology acting as a significant support in surgical settings. The platform, in use in over 30 countries, uses modular robotic arms that replicate the dexterity and precision of human hands. The system is designed for minimally invasive surgeries, including colorectal, urological, and gynecological procedures. The system’s success in performing more than 30,000 procedures also highlights its growing acceptance among hospitals and surgical teams worldwide.
Another example is that of Temi Robots in Singapore, which was initially used to prevent the spread of COVID-19 within healthcare environments. These robots, initially designed for social interaction, were repurposed to handle routine tasks like checking temperatures, delivering sanitizer, and facilitating video consultations, as shown in the image below.

Figure 10: RoboSolutions: temi Service Robots in Healthcare: 10 Use Cases in Singapore Hospitals
The robot’s capabilities significantly eased the burden on hospital staff, enabling them to focus on more critical care. The Sengkang Community Hospital used these robots during the peak of the pandemic, and they are still in use for patient engagement and triage services. Temi robots cost approximately $4,000 each and have proven effective in maintaining essential operations during staffing shortages and health crises.
Doña Paquita, a robot designed by Alicante firm Bumerania Robotics, is also being trialled at a Vitasol5 nursing home in Alicante, Spain. They note that the robot has become a “key ally in the fight against unwanted loneliness.” The robot can also measure blood pressure, heart rate, body temperature, and other vital signs, contains fall sensors to detect falls, and reminds the elderly person to take their medications on time.
Pepper, the humanoid robot developed by SoftBank, has also been used in various healthcare settings, particularly in hospitals and clinics, to guide patients and help with anxiety. Pepper is currently being used in retirement homes to test the potential of robots in the fight against the shortage of skilled nursing staff. So far, the response has been “largely positive”. Pepper was also used at Townsville Hospital in Australia, in the corner of a 16-bed emergency ward, as well as in the hospital’s main foyer, programmed to ask people about whether they had a flu shot, their attitudes towards vaccination and washing their hands to avoid disease.
Bedside Future: What’s Next in Med-Robotics
As healthcare evolves, humanoid robots are poised to redefine patient care, workforce dynamics, and global health equity. Some emerging trends highlight the ways in which these tools may continue to develop.
Importantly, medical robots are transitioning from task-specific machines to generalists capable of performing multiple roles across departments. Robots may soon be able to both assist in surgery, deliver medications, provide patient companionship, and deal with administrative tasks.
In addition, telepresence robots equipped with cameras, microphones, and screens, may increasingly allow doctors to conduct virtual consultations, monitor patients, and assist in surgeries from a distance. For example, Reachy, a humanoid robot, has been used for remote consultations and physical therapy related to prosthetic limb usage and muscle control for patients prior to being fitted with a prosthetic.
Additionally, Operation Lindbergh in 2001 demonstrated the feasibility of remote surgery, where a surgeon in New York performed a gallbladder removal on a patient in France using a ZEUS surgical robot. Recently, a surgery took place in which a Florida-based doctor performed remote surgery on a patient in Africa. As part of a transcontinental robotic telesurgery test, the surgery took place using a Medbot robot to remove prostate cancer from the man. As technology improves, these types of operations may become more commonplace.
The NHS (the British healthcare system) is already using drone and ground delivery robots to help “automate the final ‘clinical metre’ of hospital logistics.” This has been described as an “innovative way to help us care for our most vulnerable patients by speeding up test results and doing this in a way which is sustainable” by Professor Ian Abbs, chief executive of Guy’s and St Thomas NHS Foundation Trust Hospital.

Figure 11. Digital Health. NHS ground delivery robot.
In addition, Cera Care in the UK is trialling the use of robots to assist in-home care for the elderly and vulnerable, delivering over 3,000 virtual visits weekly.
Advancements in AI are also leading to the development of personalized robotic caregivers that adapt to individual patient histories, behaviors, and recovery patterns. For instance, ElliQ, an AI-powered companion robot, has been updated to monitor seniors’ health and well-being, alerting caregivers to significant changes such as poor sleep or illness. This proactive approach allows for timely interventions and supports aging in place.
While humanoid robots in healthcare were once considered glorified assistants or fancy tools, they’re now rising to the challenge as intellectual partners in the clinical environment. It’s no longer about simply executing repetitive tasks. These robots are equipped with advanced cognitive systems, acting as real-time clinical assistants, and offering insights that help guide doctors and patients toward better decisions.
For instance, some robots are being integrated with clinical decision support systems (CDSS) that combine patient records, current symptoms, medical research databases, and local hospital protocols to offer highly tailored treatment suggestions. These systems can even prioritize patients based on acuity, monitor drug interactions, and present risk-adjusted diagnostic options. In trials, robot-assisted rounds have led to faster diagnoses, fewer treatment errors, and improved documentation accuracy. Such partnerships between machines and clinicians signal a profound shift from automation to augmentation in medical care.
In the years ahead, we can expect robots to not only take the lead in providing physical assistance but also to guide clinicians and patients through complex decisions, all while keeping the “human” in healthcare. It’s safe to say, we’re headed toward a future where robots are not only saving lives, but they’re also understanding them.
Final Thoughts: Do No Harm, But Do More
Humanoid robots are poised to become a transformative force in healthcare, not by replacing doctors or nurses, but by extending their reach, reducing their workloads, and improving patient outcomes. From surgical precision to emotional intelligence, these robots bring together cutting-edge advances in AI, robotics, and human-machine interaction. They are already being used in several hospitals, nursing homes, and rehabilitation clinics around the world.
Yet, the road to widespread adoption is far from smooth. Regulatory hurdles, skepticism, infrastructure needs, and ethical debates are all difficult hurdles that need to be overcome. Hospitals need to not only think about the clinical value of humanoid robots but also prepare for workflow changes, infrastructure updates, and building trust among staff and patients.
Still, the momentum is clear: investment is growing, use cases are expanding, and the technology is rapidly maturing. The next wave of medical robotics will likely involve generalist humanoids that can switch more fluidly between roles, provide personalized care, and support medical professionals with both physical tasks, organizational issues, and decision-making.
Ultimately, success depends on how well these robots are designed with humans in mind: not just to deliver care, but to deliver it compassionately, reliably, and respectfully. If done right, humanoid robots will help to build a more efficient, high-tech, and modern healthcare system.